10 May MOH LISTEN PROCESS FOR SUSTAINABILITY THROUGH CPs
Introduction
Since 2018, the LISTEN model has been implemented in several communities in Eswatini by the Ministry of Health of the KoE and Georgetown University Center for Global Health Practice and Impact (CGHPI.
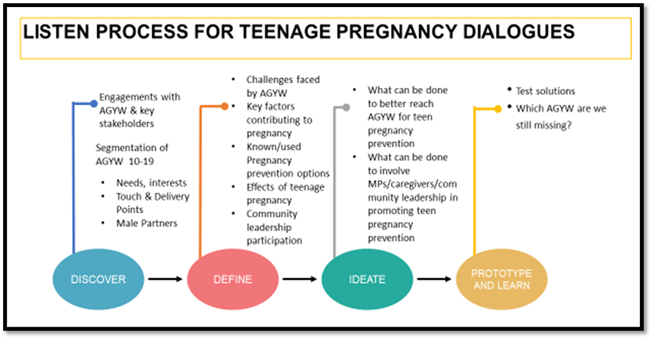
Through this approach, the LISTEN project has identified communities of practice in each implementing chiefdom where HCD is used to identify challenges and co-create sustainable solutions. In the Lobamba Lomdzala Inkhundla, the service CP which includes implementing partners and some community leadership members had a data sharing meeting where the Luyengo Clinic presented facility health data. The key focus of the presentation was on teenage pregnancy which was identified as a key issue for the community. The service CP in collaboration with the Leadership CP, initiated dialogues in the 6 zones in the community. The MOH-LISTEN project provided technical support to the CP in creating the engagement tool.
Key Insights
AGYW identified to be at risk: | Engagements with AGYWs | Engagements with parents and caregivers | Engagements with Male Partners |
|
|
|
|


No Comments